VA Enrollment Coordinator

About Veterans Desk
Veterans Desk is a 501(c)(3) nonprofit, founded by Veterans and their families. We know the system inside and out—because we’ve lived it. We’ve navigated referrals, waited on authorizations, and struggled through the endless acronyms that stand between Veterans and care.
Our mission is simple: remove the barriers that delay care.
One of the biggest barriers? Paperwork that slows down provider enrollment.
Optum and TriWest run the VA Community Care Network (CCN), but they don’t fix incomplete packets. That leaves providers on their own—and Veterans waiting.
That’s where our VA Community Care Provider Enrollment Coordinators come in. These non-medical independent contractors step in to clean up, complete, and shepherd provider documents through the process.
Why This Role is Needed
VA’s TPAs don’t fix paperwork
They only process what they’re given.
Providers are overwhelmed
They want to serve Veterans but aren’t always sure what’s required

Small errors cause big delays
A missing signature, expired license, or mismatched NPI can add weeks to approval.
Veterans pay the price
Why this role exists
Optum (Regions 1–3) and TriWest (Regions 4–5)
Manage the official portals and perform credentialing reviews.
Providers
Must upload documents, keep CAQH current, and often complete both electronic and paper submissions.
Inconsistent
If files are incomplete or inconsistent, they’re returned with a deficiency notice—slowing everything down.
Optum and TriWest
Process and review submissions, but they don’t prepare or organize a provider’s paperwork.
Plainly
Optum/TriWest
Built to process completed files and enforce network rules.
Providers
Busy, often new to dual submissions and portal nuances.
Veterans Desk Coordinators
Independent contractors who bridge the gap—helping providers organize, verify, and submit cleaner packets while keeping follow-up on track.
What our members typically handle
01
Gather and organize paperwork.
02
Quality-check for legibility, expiration dates, and consistent identifiers.
03
Anticipate both electronic and paper submission requirements.
04
Prepare cleaner packets (under provider direction).
05
Conduct recommended follow-ups (e.g., Day-7 check, Day-14 escalation).
06
Track expirations to help prevent avoidable lapses.
What Our Coordinators Do
Document Collection & QC
- W-9s, EFT/ERA, malpractice dec pages, licenses, DEA certificates, board certifications.
- Every file reviewed for legibility, expiration, and matching identifiers.
Profile Verification
- NPI records aligned with W-9 and license.
- CAQH current and shared with payers.
- Practice demographics updated.
Dual Submission Awareness
- Many forms must be uploaded and mailed.
- Members schedule, track, and proof both submissions.
Deficiency Resolution
- Catch mismatches early.
- Fix and resubmit quickly.
- Maintain proof of correction.
Renewal Tracking
- Licenses, DEA, malpractice, and board certifications tracked with 90/60/30-day reminders.
Why Providers Need This
VS
Without a Coordinator
- ❌ Enrollment is delayed.
- ❌ Deficiencies add weeks.
- ❌ Admin staff burn out.
- ❌ No billing until approved.
With a Coordinator
- First submissions are clean.
- Approvals arrive faster.
- Deficiencies resolved in days, not weeks.
- Billing begins sooner.
- Veterans access care without delays.
Comparison: Who Does What
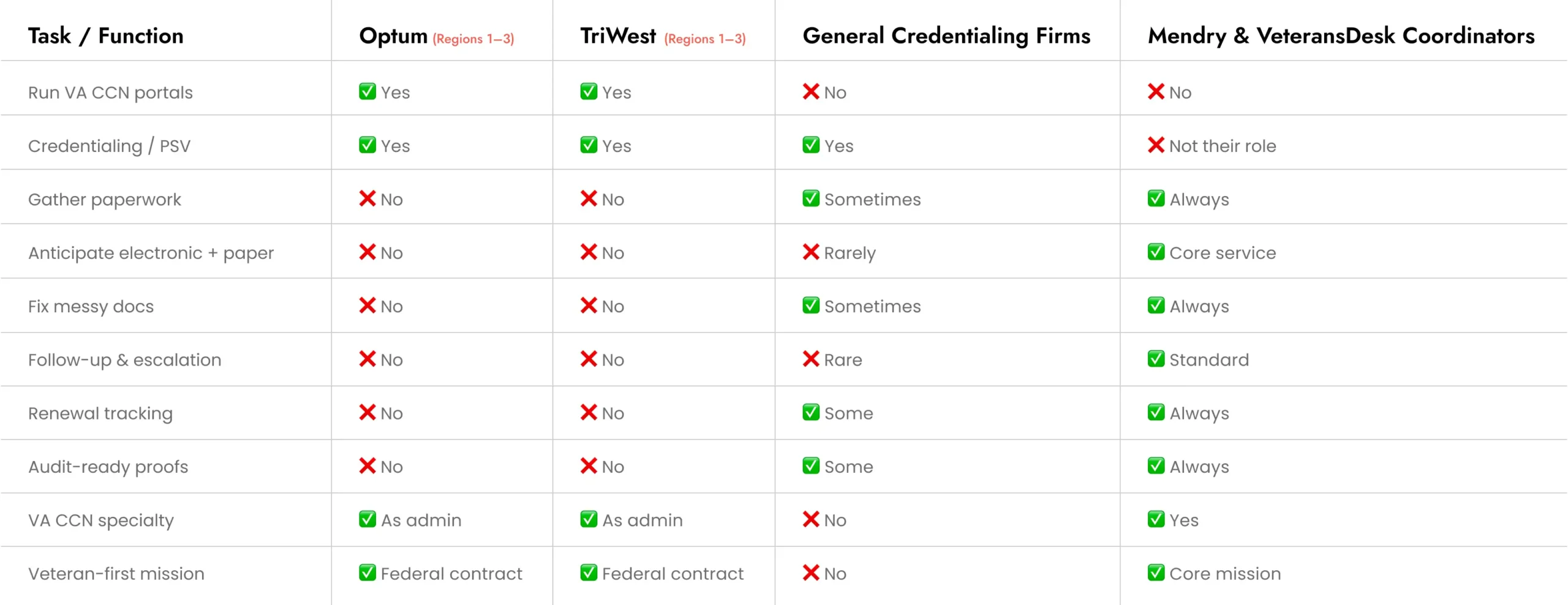

Who else provides similar help?
Optum and TriWest
Are the official administrators. They contract and activate providers, but do not manage providers’ internal paperwork.
Credentialing/enrollment firms
May support payer enrollment broadly; some overlap with these tasks, depending on scope.
VA medical centers
May offer guidance, but generally do not prepare complete enrollment packets for providers.
How our members work
01
Independent Contractors
Set their own schedules and practices while meeting Veterans Desk’s quality standards.
02
Scopes & Deadlines
03
Status Transparency
04
Professional Cadence
05
Audit-Ready Files
become a enrolment coordinator At Veterans Desk
Tier 3
Enrollment Coordinator Partner
$50/month/
See More
- Everything in Tier 2
- Dedicated provider spotlight feature
- Co-branding on Mendry events/pods
- Social media amplification through Mendry channels
Perfect for:
Veteran-focused providers ready to grow their outreach, educate on VA care topics, and actively engage with the community.
VA Enrollment Coordinators Providers
Why Veterans Desk
Veterans Desk mission is to help providers navigate enrollment paperwork more efficiently, reducing common delays and supporting quicker access to care for Veterans.

Compliance guardrails
Strictly administrative, non-medical, PHI-light, no clinical advice.

Community strength
Independent contractors share tools and templates through a nonprofit-supported network.

Scalability
From single clinics to large practices, Coordinators adapt quickly to demand.
This is an illustrative example. Timelines and outcomes vary by region, volume, and payer processing.
Ready to Serve Veterans Faster?
If you’re a provider joining VA CCN—or an administrator aiming to streamline your paperwork pipeline—Veterans Desk can connect you with a VA Community Care Provider Enrollment Coordinator.
- Organized, submission-ready packets
- Anticipated electronic + paper steps
- Documented follow-ups and escalation
- Renewal tracking and audit-friendly records
Each role has its lane
Optum and TriWest administer and process, providers supply complete documentation, and Veterans Desk Coordinators step in to make the paperwork cleaner, timelier, and easier to manage.